The truth about Inductions
Sometimes it is better to help get labor started. Our bodies aren’t perfect at knowing the right time and sometimes it’s better for babies not to have to rely on a placenta. After 39 weeks labor has few risks. It does increase pain/perception of pain because you are stuck in the hospital, tied to machines It is unpredictable. I can’t tell you if it is going to take 5 minutes or 5 days to get your body to start the labor process. All I can do is try and get labor started.
Why?
There are a number of reasons why we may decide to induce labor, including,
- you’re overdue. If there’s no sign of action from your uterus, your practitioner may induce you around 41-42 weeks, this is because after 42 weeks the placenta wears out and babies start to lose weight and get tired.
- There’s a complication. Sometimes conditions like preeclampsia, diabetes, gestational diabetes, issues with the placenta, or problems with amniotic fluid (low levels or infection) make it risky to continue the pregnancy.
- Your membranes ruptured. If your water has broken and contractions have not started on their own within 24 hours, your doctor may induce.
- Your baby isn’t thriving. If tests suggest your baby is mature enough to deliver, your practitioner may opt for induction.
- You live far from the hospital. You may be induced if you live far from where you’re delivering or have had previous short labor because there’s concern that you might not make it to the hospital or birthing center in time. Known as an elective induction, it should be scheduled at the place where you plan to deliver no earlier than 39 weeks.
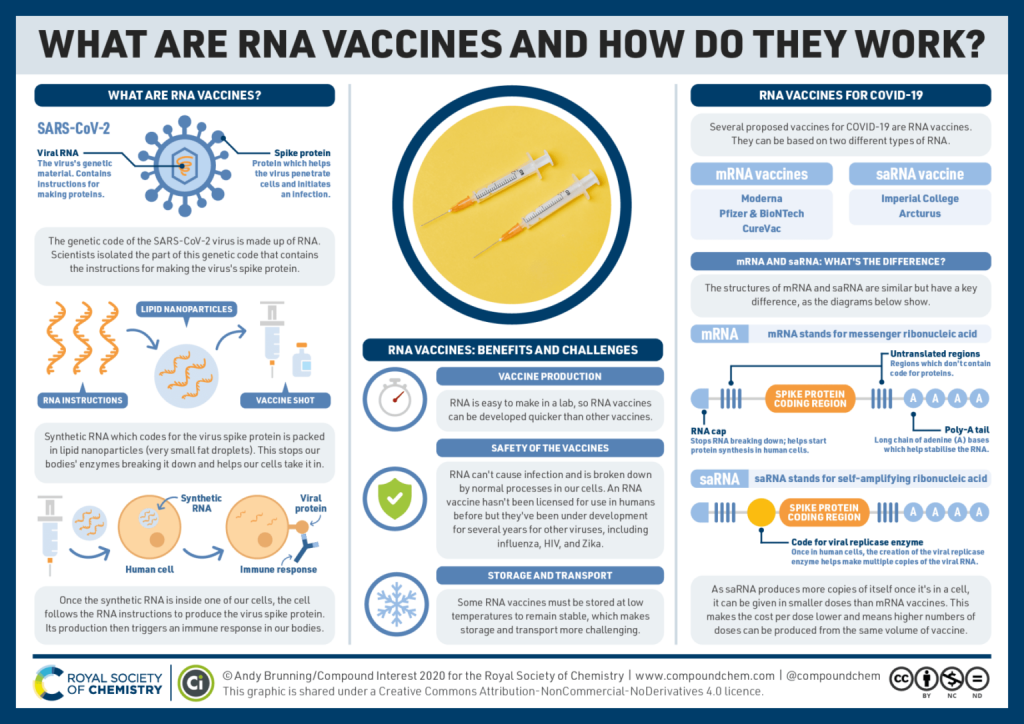
How does labor induction work?
If you do end up needing to be induced, the process involves a number of steps, though you usually won’t go through all of them:
• Cervical ripening. Usually, your cervix will open up naturally on its own once you’re ready to go into labor. However if your cervix shows no signs of dilating and effacing (softening, opening, thinning) to allow your baby to leave the uterus and enter the birth canal, your practitioner will need to get the ripening rolling. She’ll usually do this by applying a topical form of the hormone prostaglandin (either a gel or a vaginal suppository) to your cervix. Your cervix will be checked after a few hours; often, this will be enough to get labor and contractions started. However if the prostaglandin is doing its work ripening the cervix but contractions haven’t started, the process continues on to the following steps. (Note that sometimes if you’ve had a C-section or other previous uterine surgery, you won’t be given prostaglandin to try to prevent uterine rupture. And in some cases, your practitioner may use a mechanical agent to ripen the cervix, such as a catheter with an inflatable balloon or graduated dilators, instead.)
• Rupturing the membrane. If your cervix has already begun to dilate and efface on its own but your water hasn’t broken, your practitioner might jump-start your contractions by artificially rupturing the membranes. In other words, she’ll break the bag of waters that surrounds your baby manually using an instrument that looks like a long crochet hook with a sharp tip. It might feel uncomfortable, but it shouldn’t be painful. This is one of the procedures that the new ACOG guidelines suggest may not be necessary for all women with low-risk pregnancies.
• Pitocin. If neither the prostaglandin gels nor the stripping nor rupturing of the membranes has brought on regular contractions within a couple of hours, your practitioner will slowly give you the medication Pitocin (a synthetic form of the naturally-occurring hormone oxytocin) via an IV to induce or augment contractions. When Pitocin is used, contractions — which usually start about 30 minutes later — are usually stronger, more regular, and more frequent than those where labor has begun naturally (though if this is your first baby, you won’t have anything to compare it with). If you’re considering an epidural, you might want to ask your practitioner about getting it started while you’re getting the Pitocin so it’s in place once labor does start.
The risks of labor induction
While in the majority of cases labor induction goes smoothly, complications sometimes arise. They include:
- Inductions increase pain because you are stuck in the hospital, and can’t move around naturally.
- Inductions are unpredictable, you might get stuck in the hospital for several days before we get labor started
- Fetal stress, we monitor the baby the whole time you are in labor and sometimes artificial contractions can stress the baby out. Studies have shown that babies do not have any long term risks/stress, but temporary fetal stress is stressful
- Increase stress on your body.
- Increase stress on your body.
- Bleeding after delivery
- Inductions do not increase the risk of cesarean section. Many studies have shown that earlier inductions do not increase this risk.
Do-it-yourself labor induction
While there are plenty of natural methods you can use to try to bring on labor (and plenty of old wives’ tales to go along with them), none of them have been shown to work more than placebo pills. After 39 weeks no matter what happens you will eventually go into labor on your own, and if you want to wait, and your baby is doing well….you can wait.