This post was made by the Mayo Clinic and it is just general information:
Overview
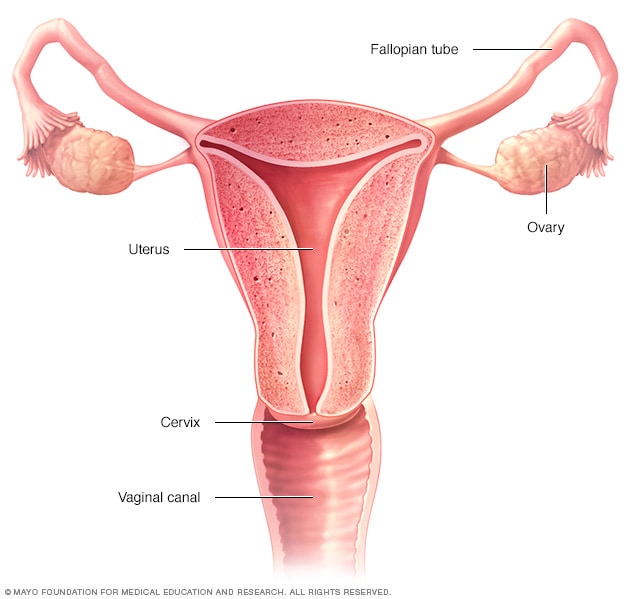 Female reproductive systemOpen pop-up dialog box
Female reproductive systemOpen pop-up dialog box
Vaginal hysterectomy is a surgical procedure to remove the uterus through the vagina.
During a vaginal hysterectomy, the surgeon detaches the uterus from the ovaries, fallopian tubes and upper vagina, as well as from the blood vessels and connective tissue that support it, before removing the uterus.
Vaginal hysterectomy involves a shorter time in the hospital, lower cost and faster recovery than an abdominal hysterectomy, which requires an incision in your lower abdomen. However, depending on the size and shape of your uterus or the reason for the surgery, vaginal hysterectomy might not be possible. Your doctor will talk to you about other surgical options, such as an abdominal hysterectomy.
Hysterectomy often includes removal of the cervix as well as the uterus. When the surgeon also removes one or both ovaries and fallopian tubes, it’s called a total hysterectomy with salpingo-oophorectomy (sal-ping-go-o-of-uh-REK-tuh-me). All of these organs are part of your reproductive system and are situated in your pelvis.
Why it’s done
Vaginal hysterectomy treats various gynecological problems, including:
- Fibroids. Many hysterectomies are done to permanently treat these benign tumors in your uterus that can cause persistent bleeding, anemia, pelvic pain, pain during intercourse and bladder pressure. For large fibroids, you might need surgery that removes your uterus through an incision in your lower abdomen (abdominal hysterectomy).
- Endometriosis. This occurs when the tissue lining your uterus (endometrium) grows outside the uterus, involving the ovaries, fallopian tubes or other organs. Most women with endometriosis have a laparoscopic or robotic hysterectomy or abdominal hysterectomy, but sometimes a vaginal hysterectomy is possible.
- Adenomyosis. This occurs when the tissue that normally lines the uterus grows into the uterine wall. An enlarged uterus and painful, heavy periods result.
- Gynecological cancer. If you have cancer of the uterus, cervix, endometrium or ovaries, or precancerous changes, your doctor might recommend a hysterectomy. Most often, treatment for ovarian cancer involves an abdominal hysterectomy, but sometimes vaginal hysterectomy is appropriate for women with cervical or endometrial cancer.
- Uterine prolapse. When pelvic supporting tissues and ligaments weaken or stretch out, the uterus can sag into the vagina, causing urine leakage, pelvic pressure or difficulty with bowel movements. Removing the uterus and repairing supportive tissues might relieve those symptoms.
- Abnormal uterine bleeding. When medication or a less invasive surgical procedure doesn’t control irregular, heavy or very long periods, hysterectomy may be needed.
- Chronic pelvic pain. If your pain is clearly caused by a uterine condition, hysterectomy might help, but only as a last resort. Chronic pelvic pain can have several causes, so an accurate diagnosis of the cause is critical before having a hysterectomy.
For most of these conditions — with the possible exception of cancer — hysterectomy is just one of several treatment options. You might not need to consider hysterectomy if medications or less invasive gynecological procedures manage your symptoms.
You cannot become pregnant after a hysterectomy. If you’re not sure that you’re ready to give up your fertility, explore other treatments.
Risks
Although vaginal hysterectomy is generally safe, any surgery has risks. Risks of vaginal hysterectomy include:
- Heavy bleeding
- Blood clots in the legs or lungs
- Infection
- Damage to surrounding organs
- Adverse reaction to anesthetic
Severe endometriosis or scar tissue (pelvic adhesions) might force your surgeon to switch from vaginal hysterectomy to laparoscopic or abdominal hysterectomy during the surgery.
How you prepare
As with any surgery, it’s normal to feel nervous about having a hysterectomy. Here’s what you can do to prepare:
- Gather information. Before the surgery, get all the information you need to feel confident about it. Ask your doctor and surgeon questions.
- Follow your doctor’s instructions about medication. Find out whether you should take your usual medications in the days before your hysterectomy. Be sure to tell your doctor about over-the-counter medications, dietary supplements or herbal preparations that you take.
- Discuss anesthesia. You might prefer general anesthesia, which makes you unconscious during surgery, but regional anesthesia — also called spinal block or epidural block — might be an option. During a vaginal hysterectomy, regional anesthesia will block the feelings in the lower half of your body. With general anesthesia, you’ll be asleep.
- Arrange for help. Although you’re likely to recover sooner after a vaginal hysterectomy than after an abdominal one, it still takes time. Ask someone to help you out at home for the first week or so.
What you can expect
Talk with your doctor about what to expect during and after a vaginal hysterectomy, including physical and emotional effects.
During the procedure
You’ll lie on your back, in a position similar to the one you’re in for a Pap test. You might have a urinary catheter inserted to empty your bladder. A member of your surgical team will clean the surgical area with a sterile solution before surgery.
To perform the hysterectomy:
- Your surgeon makes an incision inside your vagina to get to the uterus
- Using long instruments, your surgeon clamps the uterine blood vessels and separates your uterus from the connective tissue, ovaries and fallopian tubes
- Your uterus is removed through the vaginal opening, and absorbable stitches are used to control any bleeding inside the pelvis
Except in cases of suspected uterine cancer, the surgeon might cut an enlarged uterus into smaller pieces and remove it in sections (morcellation).
Laparoscopic or robotic hysterectomy
You might be a candidate for a laparoscopically assisted vaginal hysterectomy (LAVH) or robotic hysterectomy. Both procedures allow your surgeon to remove the uterus vaginally while being able to see your pelvic organs through a slender viewing instrument called a laparoscope.
Your surgeon performs most of the procedure through small abdominal incisions aided by long, thin surgical instruments inserted through the incisions. Your surgeon then removes the uterus through an incision made in your vagina.
Your surgeon might recommend LAVH or robotic hysterectomy if you have scar tissue on your pelvic organs from prior surgeries or from endometriosis.
After the procedure
After surgery, you’ll be in a recovery room for one to two hours and in the hospital overnight. Some women are able to go home the day of the surgery.
You’ll take medication for pain. Your health care team will encourage you to get up and move as soon as you’re able.
It’s normal to have bloody vaginal discharge for several days to weeks after a hysterectomy, so you’ll need to wear sanitary pads.
How you’ll feel physically
Recovery after vaginal hysterectomy is shorter and less painful than it is after an abdominal hysterectomy. A full recovery might take three to four weeks.
Even if you feel recovered, don’t lift anything heavy — more than 20 pounds (9.1 kilograms) — or have vaginal intercourse until six weeks after surgery.
Contact your doctor if pain worsens or if you develop nausea, vomiting or bleeding that’s heavier than a menstrual period.
How you’ll feel emotionally
After a hysterectomy, you might feel relief because you no longer have heavy bleeding or pelvic pain.
For most women, there’s no change in sexual function after hysterectomy. But for some women, heightened sexual satisfaction occurs after hysterectomy — perhaps because they no longer have pain during intercourse.
You might feel a sense of loss and grief after hysterectomy, which is normal. Or you might have depression related to the loss of your fertility, especially if you’re young and hoped for a future pregnancy. If sadness or negative feelings interfere with your enjoyment of everyday life, talk to your doctor.
Results
After a hysterectomy, you’ll no longer have periods or be able to get pregnant.
If you had your ovaries removed but hadn’t reached menopause, you’ll begin menopause immediately after surgery. You might have symptoms such as vaginal dryness, hot flashes and night sweats. Your doctor can recommend medications for these symptoms. Your doctor might recommend hormone therapy even if you don’t have symptoms.
If your ovaries weren’t removed during surgery — and you still had periods before your surgery — your ovaries continue producing hormones and eggs until you reach natural menopause.

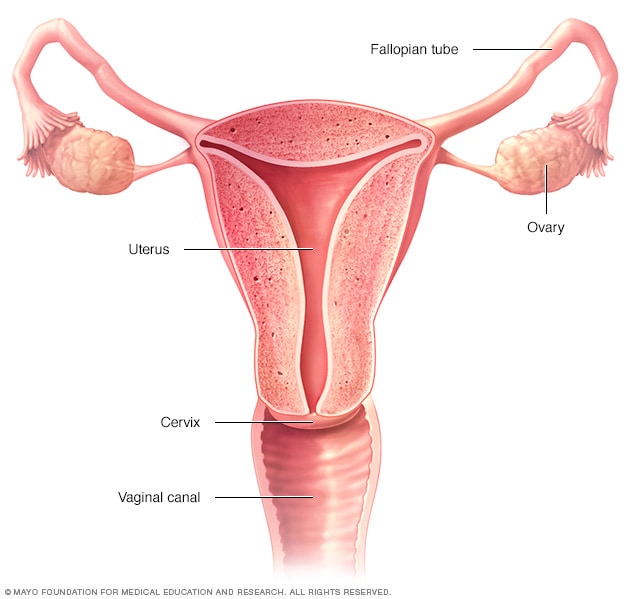 Female reproductive systemOpen pop-up dialog box
Female reproductive systemOpen pop-up dialog box